What Is T-DM1 And What Is It Used For?
18-20% of metastatic breast cancers are HER-2 +, that is, they show overexpression of the HER2 oncogene. A new drug T-DM1 has been developed to treat this type of tumor. Let’s see what it is.
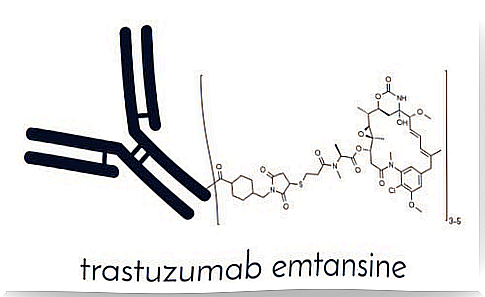
T-DM1 is a new, unique and selective antineoplastic drug approved by the EMA for the treatment of advanced HER-2 positive breast cancer. HER-2 is a protein known as “epidermal growth factor receptor 2”. It promotes the growth of cancer cells. It is found commercially under the name Kadcyla .
The T-DM1 consists of two parts. One is the medicine already known as trastuzumab, which is an anti-HER2 antibody. And the other is an antimicrobial cytotoxic molecule – DM1. The fact that it is a cytotoxic anti-microtubule refers to its ability to block the synthesis of microtubules during cell division, a mechanism that we will see in detail later.
Effectiveness of T-DM1

18-20% of metastatic breast cancers are HER-2 +. In other words, they are characterized by overexpression and / or amplification of the HER2 oncogene. Before the development of specific anti-HER2 therapies, the prognosis of patients with HER-2 + tumors was significantly worse than that of others.
An oncogene is a gene whose mutation or transformation capacity induces the formation of cancer in a cell.
However, with the development of trastuzumab, approved in 2000, the poor prognosis for HER2 + breast cancer compared to HER2- was countered.
In 2014, a second anti-HER2 drug was released to the market. This is pertuzumab. The latter drug further prolongs overall survival in the first-line treatment of advanced HER2 + breast cancer.
As for the second-line treatment for advanced HER2 + breast cancer, the only one approved to date was a combination of chemotherapy with capecitabine plus lapatinib – an HER2 / ERGFR tyrosine kinase inhibitor.
A registry study called EMILIA compared treatment with T-DM1 with treatment with lapatinib plus capecitabine in patients with this type of breast cancer who had previously been treated with trastuzumab plus a taxane.
The results of this study showed an increase in progression-free survival, an increase in overall survival and a better tolerated side effect profile as well as a significant delay in symptoms over time until progression with treatment with T-DM1.
Mechanism of action: how does T-DM1 affect the body?
As we mentioned above, T-DM1 is formed by the combination of two drugs: trastuzumab and DM1. T-DM1 combines the mechanisms of action of these two drugs:
- Like trastuzumab, T-DM1 is able to bind to HER2 and block the growth of tumor cells that overexpress this growth factor.
- It also has the mechanism of action of DM1, i.e. it is able to bind to tubulin
By inhibiting tubulin, it stops the cancer cell from dividing. This ultimately results in the death of the cell by apoptosis. The results of in vitro cytotoxicity tests show that DM1 is 20 to 200 times more potent than taxanes and Vinca alkaloids.
Adverse effects of T-DM1
Adverse drug reactions are all unwanted and unintended effects that occur as expected with treatment with a drug.
The most frequently reported side effects were nausea, fatigue and headache. They were experienced by ≥25% of patients. In this sense, the safety of T-DM1 has been evaluated in a total of 1871 breast cancer patients in different clinical trials and it was observed that the most common serious reactions were:
- Hemorrhage
- Dyspnea
- Bone and muscle pain
- Abdominal pain
- Thrombocytopenia
- Vomiting
Conclusion
The data reported by the studies show that T-DM1 is a very relevant breakthrough in the treatment of advanced HER2 + breast cancer. It produces improved survival in patients previously treated with trastuzumab.
However, despite these advances, HER2 + metastatic disease remains incurable. We must therefore find new therapies that are more effective and better tolerated. It is therefore essential to continue active research on breast cancer.