What Is Hemispherectomy?
Hemispherectomy mainly occurs in young children because their brains have greater plasticity. The healthy cerebral hemisphere can therefore take on many of the tasks that the withdrawn hemisphere performed.
Hemispherectomy is a surgical procedure performed to treat various compulsive disorders. It is practiced when this type of disease does not respond well to another type of less radical treatment.
Everything indicates that the first hemispherectomy was performed on a dog in 1888. The first reference for this intervention in humans dates from 1923. In the 60s and 70s, several interventions of this type were performed, but they had not very encouraging results.
Currently, traditional hemispherectomy is often replaced by functional hemispherectomy. Indeed, it is a more precise and a little less invasive intervention. The success rate is much higher than in the past.
What is hemispherectomy?
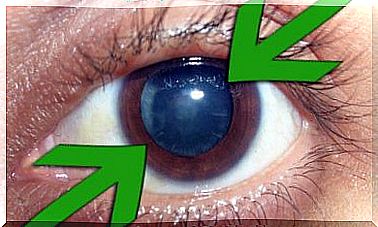
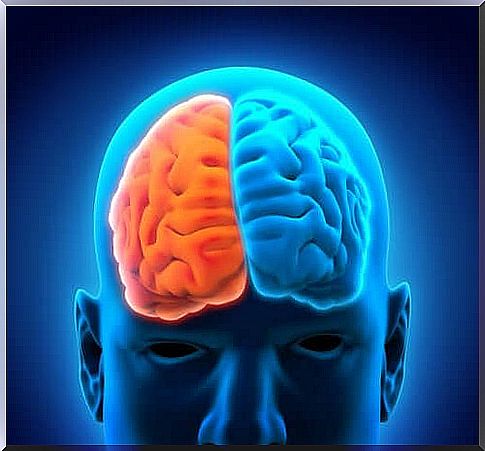
Hemispherectomy is a neurosurgical procedure that involves removing one of the hemispheres of the brain. Sometimes it’s the right and other times it’s the left. It is mainly practiced in children between 5 and 10 years old.
This type of intervention is mainly used as an anti-convulsive treatment. However, it is also performed in certain patients with neurological deficit and exceptionally in cases of severe head trauma.
Although it is customary to remove the entire cerebral hemisphere, sometimes it is sufficient to remove only one part. In this case, it is called a functional hemispherectomy. Therefore, if a tiny part of the damaged tissue is left behind, the seizure disorder may reappear.
Indications
In general, hemispherectomy is indicated for patients with continuous, daily seizures. And who have not responded to pharmacological treatment or other type of less invasive surgical procedures.
This surgical intervention is indicated in the following cases:
- Infantile hemiplegia: only for children over 4 years old with convulsive and mental disorders. And after checking for 2 years that the individual does not react to pharmacological treatment
- Sturge-Weber Syndrome: This is a neuro-cutaneous disorder characterized by a facial stain in the area of the trigeminal nerve. Intervention is indicated when seizures start very early and the disorder involves the entire hemisphere
- Rasmussen syndrome: it is a brain disorder that generates chronic and progressive encephalitis. It is better to intervene as soon as possible
- Hemimegalencephaly: this is an inflammatory and rare neurological disease characterized by severe seizures. The operation, in this case, is still a source of debate.
- Cortical development abnormalities: only when hemispherical malformations are unilateral
Characteristics of intervention methods
There are 4 procedures for hemispherectomy. But in each of them, success depends on controlling hemostasis. Here are the other methods:
- Anatomical hemispherectomy
- Hemidecortication
- Functional hemispherectomy
- Modified functional hemispherectomy
The typical procedure is performed under general anesthesia. It begins with the shaving of the head and the demarcation of the incision lines. Then the cut is made and the dura is exposed and removed to see the brain.
When the brain is visible, the part that will be removed is marked. Then we take it out, cauterize the blood vessels and place a drain. Finally, the reverse procedure is performed. Namely, the dura mater, bones and scalp are put back in their place. The incision is sewn up with staples.
The post-operative hemispherectomy
This type of post-operative is very painful. Usually, the drain tube remains in place for 3 or 4 days and then assesses its possible removal. However, before removing it, it is very important to perform diagnostic tests on the case to assess whether there is any bleeding or hemorrhaging.
The main immediate postoperative complications are related to hemodynamic instability, hypothermia and hypo or hyperkalaemia. Normally this is successfully controlled in the Intensive Care Unit.
The onset of seizures early in the postoperative period is considered a serious complication. Hydrocephalus occurs in almost half of the cases and almost all patients develop aseptic meningitis. In addition, the mortality rate fluctuates between 4% and 6%.
Finally, between 70 and 85% of patients undergoing a hemispherectomy succeed in controlling their seizures. About 10-20% significantly improve their quality of life. However, there is some evidence that some complications can appear late.